







Inflammation is part of healing — but when it drags on, it causes pain and slows repair. HBOT delivers concentrated oxygen that helps your body settle inflammation naturally. It reduces the chemicals that drive swelling while improving blood flow and tissue repair.
More oxygen allows your body to clear waste and calm irritation faster. HBOT has been shown to lower inflammation markers and promote faster recovery from surgery, injury, and strenuous training. It’s a simple way to support comfort and recovery without relying on medication.
(For clinicians and advanced readers)
Meng XE, Zhang Y, Li N, et al. Hyperbaric oxygen alleviates secondary brain injury after trauma through inhibition of TLR4/NF-κB signaling pathway. Med Sci Monit. 2016;22:284–288. Published 2016 Jan 26. doi:10.12659/msm.894148
Dulai PS, Gleeson MW, Taylor D, et al. (2014), Systematic review: the safety and efficacy of hyperbaric oxygen therapy for inflammatory bowel disease. Aliment Pharmacol Ther, 39: 1266-1275. doi:10.1111/apt.12753
Hui J, Zhang ZJ, Zhang X, et al. Repetitive hyperbaric oxygen manage attenuates complete Freund’s adjuvant-induced pain and reduces glia-mediated neuroinflammation in the spinal cord, J. Pain, 14 (7) (2013), pp. 747-758
Li F, Fang L, Huang S, et al. Hyperbaric oxygenation therapy alleviates chronic constrictive injury-induced neuropathic pain and reduces tumor necrosis factor-alpha production. Anesth. Analg., 113 (3) (2011), pp. 626-633
Choudhury R. Hypoxia and hyperbaric oxygen therapy: a review. Int J Gen Med. 2018;11:431–442. Published 2018 Nov 20. doi:10.2147/IJGM.S172460
He H, Li X, He Y. Hyperbaric oxygen therapy attenuates neuronal apoptosis induced by traumatic brain injury via Akt/GSK3β/β-catenin pathway. Neuropsychiatr Dis Manage. 2019;15:369–374. Published 2019 Jan 25. doi:10.2147/NDT.S183632
Wu HH, Huang CC, Chang CP, et al. Heat shock protein 70 (HSP70) reduces hepatic inflammatory and oxidative damage in a rat model of liver ischemia/reperfusion injury with hyperbaric oxygen preconditioning. Med Sci Monit. 2018;24:8096–8104. Published 2018 Nov 12. doi:10.12659/MSM.911641
Thompson CD, Uhelski ML, Wilson JR, et al. Hyperbaric oxygen manage decreases pain in two nerve injury models. Neurosci. Res., 66 (3) (2010), pp. 279-283
Oyaizu T, Enomoto M, Yamamoto N, et al. Hyperbaric oxygen reduces inflammation, oxygenates injured muscle, and regenerates skeletal muscle via macrophage and satellite cell activation. Sci Rep. 2018;8(1):1288. Published 2018 Jan 22. doi:10.1038/s41598-018-19670-x
Zhao BS, Meng LX, Ding YY, et al. Hyperbaric oxygen manage produces an antinociceptive response phase and inhibits astrocyte activation and inflammatory response in a rat model of neuropathic pain. J. Mol. Neurosci., 53 (2) (2014), pp. 251-261
Novak S, Drenjancevic I, Vukovic R, et al. Anti-inflammatory effects of hyperbaric oxygenation during DSS-induced colitis in BALB/c mice include changes in gene expression of HIF-1α, proinflammatory cytokines, and antioxidative enzymes. Mediators Inflamm. 2016;2016:7141430. doi:10.1155/2016/7141430
Hou S, Wu G, Liang J, et al. Hyperbaric oxygen on rehabilitation of brain tumors after surgery and effects on TNF-α and IL-6 levels. Oncol Lett. 2019;17(3):3277–3282. doi:10.3892/ol.2019.10000
Di Sabato F, Rocco M, Martelletti P, et al. Hyperbaric oxygen in chronic cluster headaches: influence on serotonergic pathways. Undersea Hyperb. Med., 24 (2) (1997), pp. 117-122
Bennett MH, French C, Schnabel A, et al. Normobaric and hyperbaric oxygen therapy for migraine and cluster headache. Cochrane Database Syst. Rev. (3)(2008).
Fosen KM, Thom SR. Hyperbaric oxygen, vasculogenic stem cells, and wound healing. Antioxid Redox Signal. 2014;21(11):1634–1647. doi:10.1089/ars.2014.5940
Every cell in your body runs on energy made from oxygen. When you’re stressed, injured, or tired, those energy systems slow down. HBOT increases oxygen in the bloodstream, helping your cells produce more of the energy they need to heal, think, and move.
With more oxygen to work with, cells can recover faster and perform better. Studies show HBOT boosts energy production, supports stem-cell activity, and reduces oxidative stress. Over time, that can mean better focus, quicker recovery, and more sustained physical and mental energy.
(For clinicians and advanced readers)
Palzur E, Zaaroor M, Vlodavsky E, et al. Neuroprotective effect of hyperbaric oxygen therapy in brain injury is mediated by preservation of mitochondrial membrane properties. Brain Res., 1221 (2008), pp. 126-133
K.R. Dave, R. Prado, R. Busto, A.P. Raval, W.G. Bradley, D. Torbati, M.A. Pérez-pinzón,
Hyperbaric oxygen therapy protects against mitochondrial dysfunction and delays onset of motor neuron disease in wobbler mice, Neuroscience, Volume 120, Issue 1, 2003, Pages 113-120,
ISSN 0306-4522, https://doi.org/10.1016/S0306-4522(03)00244-6.
Meyer JN, Hartman JH, Mello DF. Mitochondrial toxicity. Toxicological Sciences, Volume 162, Issue 1, March 2018, Pages 15–23.
Meyer JN, Leung MC, Rooney JP, et al. Mitochondria as a target of environmental toxicants. Toxicol Sci. 2013;134(1):1–17. doi:10.1093/toxsci/kft102
Your immune system needs oxygen to fight infection and repair damage efficiently. HBOT increases oxygen in the blood, giving white blood cells the power to kill bacteria and remove waste while reducing excess inflammation. It also activates stem cells and growth factors that rebuild damaged tissue.
HBOT strengthens your natural defence and repair systems. Clinical research shows it improves wound closure, helps fight infection, and supports new blood-vessel growth in oxygen-starved tissues. It’s a proven hospital therapy for stubborn wounds and a powerful recovery aid in wellness settings.
(For clinicians and advanced readers)
Çimşit M, Uzun G, Yıldız S. Hyperbaric oxygen therapy as an anti-infective agent. Expert Rev Anti Infect Ther. 2009;7(8):1015–1026.
Memar MY, Yekani M, Alizadeh N, et al. Hyperbaric oxygen therapy: antimicrobial mechanisms and clinical application for infections. Biomed Pharmacother. 2019;109:440–447.
Mader JT, Brown GL, Guckian JC, et al. A mechanism for the amelioration by hyperbaric oxygen of experimental staphylococcal osteomyelitis in rabbits. J Infect Dis. 1980;142(6):915–922.
Fosen KM, Thom SR. Hyperbaric oxygen, vasculogenic stem cells, and wound healing. Antioxid Redox Signal. 2014;21(11):1634–1647.
Health Quality Ontario. Hyperbaric oxygen therapy for the management of diabetic foot ulcers: a health technology assessment. Ont Health Technol Assess Ser. 2017;17(5):1–142.
Oyaizu T, Enomoto M, Yamamoto N, et al. Hyperbaric oxygen reduces inflammation, oxygenates injured muscle, and regenerates skeletal muscle via macrophage and satellite cell activation. Sci Rep. 2018;8(1):1288.

Your brain never stops adapting — it constantly builds new connections to learn, think, and remember. Hyperbaric oxygen therapy (HBOT) gives your brain extra oxygen, helping nerve cells get the fuel they need to repair and grow. This can support clearer thinking, better focus, and faster recovery after injury or illness.
By improving blood flow and giving neurons more oxygen, HBOT helps the brain “wake up” sluggish areas and strengthen communication between cells. Studies show improvements in memory, attention, and reaction time in older adults and people recovering from brain injuries. It’s a natural way to help the brain restore balance and function at its best.
(For clinicians and advanced readers)
Efrati S, Fishlev G, Bechor Y, et al. Hyperbaric oxygen induces late neuroplasticity in post stroke patients–randomized, prospective trial. PLoS One. 2013;8(1):e53716.
Boussi-Gross R, Golan H, Fishlev G, et al. Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury – randomized prospective trial. PLoS One. 2013;8(11):e79995.
Vadas D, Kalichman L, Hadanny A, et al. Hyperbaric oxygen environment can enhance brain activity and multitasking performance. Front Integr Neurosci. 2017;11:25.
Thom SR. Hyperbaric oxygen: its mechanisms and efficacy. Plast Reconstr Surg. 2011;127(Suppl 1):131S–141S.
Tal S, Hadanny A, Sasson E, et al. Hyperbaric oxygen therapy can induce angiogenesis and regeneration of nerve fibers in traumatic brain injury patients. Front Hum Neurosci. 2017;11:508.

Collagen is what keeps your skin, muscles, and joints strong — it’s the body’s built-in scaffolding. HBOT supports collagen production by flooding tissues with oxygen and activating the cells that rebuild connective tissue. It also helps tiny new blood vessels form, bringing more nutrients to healing areas.
More oxygen means faster, stronger repair. HBOT speeds up wound healing, helps grafts and skin repairs take hold, and supports post-surgery recovery by improving collagen quality and strength. It’s widely used in hospitals for slow-healing wounds and increasingly explored in recovery and cosmetic settings.
(for clinicians and advanced readers)
Bhutani S, Vishwanath G. Hyperbaric oxygen and wound healing. Indian J Plast Surg. 2012;45(2):316–324.
Fosen KM, Thom SR. Hyperbaric oxygen, vasculogenic stem cells, and wound healing. Antioxid Redox Signal. 2014;21(11):1634–1647.
Oyaizu T, Enomoto M, Yamamoto N, et al. Hyperbaric oxygen reduces inflammation, oxygenates injured muscle, and regenerates skeletal muscle via macrophage and satellite cell activation. Sci Rep. 2018;8(1):1288.
Perren S, Gatt A, Papanas N, et al. Hyperbaric oxygen therapy in ischaemic foot ulcers in type 2 diabetes: a clinical trial.
Health Quality Ontario. Hyperbaric oxygen therapy for the management of diabetic foot ulcers: a health technology assessment. Ont Health Technol Assess Ser. 2017;17(5):1–142.
Eskes AM, Ubbink DT, Lubbers MJ, et al. Hyperbaric oxygen therapy: solution for difficult to heal acute wounds? Systematic review. World J Surg. 2011;35(3):535–542.
Fujita N, Ono M, Tomioka T, et al. Effects of hyperbaric oxygen at 1.25 atmospheres absolute with normal air on macrophage number and infiltration during rat skeletal muscle regeneration. PLoS One. 2014;9(12):e115685.

Lingering inflammation can make you sore and slow down healing. Red light therapy helps calm that response by improving circulation and supporting your body’s natural antioxidant defences.
With better blood flow and less cellular stress, pain and swelling ease more quickly. Studies show red light therapy reduces soreness after exercise, speeds tissue recovery, and helps your body return to balance — naturally, without medication.
(for clinicians and advanced readers)
Marashian SM, Hashemian MR, Pourabdollah M, et al. Photobiomodulation improves serum cytokine response in mild to moderate COVID-19: The first randomized, double-blind, placebo-controlled, pilot study. Frontiers in Immunology. 2022;13:929837. Published July 8, 2022.
Zwiri AMA, Ahmad WMAW, Asif JA, et al. A randomized controlled trial evaluating the biomarkers hs‑CRP, IL‑6, and IL‑8 in patients with temporomandibular disorder treated with LLLT, conservative therapy, and combination therapy. International Journal of Environmental Research and Public Health. 2022;19(15):8987. Published July 23, 2022.
Lim W, Lee S, Kim I, et al. Photobiomodulation suppresses neuroinflammation and attenuates symptoms in chronic neuropathic pain: A randomized, placebo-controlled trial. Pain Medicine. 2023;24(5):979–988. Published May 2023
Nunes EC, Nascimento DP, Silva Júnior HD, et al. Effectiveness of photobiomodulation therapy in the management of pain and inflammation after dental implant surgery: a randomized single-blind clinical trial. J Clin Med. 2022;13(19):5709. Published October 1 2022.
de Oliveira BP, de Almeida LM, Leal-Junior ECP, et al. Effects of infrared low-level laser therapy applied prior to an intense progressive running test on inflammatory and oxidative stress markers in high-level soccer players: a randomized, triple-blind, crossover trial. Oxid Med Cell Longev. 2019;2019:6239058. Published December 5 2019.
Every cell in your body needs energy to function. Red and near-infrared light act like a natural spark, helping your cells make more of it. When light reaches your tissues, it supports the tiny “power centres” inside each cell, improving how efficiently your body produces and uses energy.
More cell energy means more vitality. Red light therapy can improve endurance, speed recovery, and enhance focus — all by helping your body’s energy systems run more smoothly. It’s a safe, non-invasive way to boost performance and resilience.
(for clinicians and advanced readers)
Fritsch CG, Dornelles MP, Teodoro JL, et al. Effects of photobiomodulation therapy associated with resistance training in elderly men: a randomized double-blinded placebo-controlled trial. Eur J Appl Physiol. 2019;119(1):279–289. Published 2018 Oct 26.
Tomazoni SS, Monteiro Machado CS, De Marchi T, et al. Infrared low-level laser therapy (photobiomodulation) before an intense progressive running test in high-level soccer players: randomized, triple-blind, crossover trial. Oxid Med Cell Longev. 2019;2019:6239058. Published 2019 Dec 5.
Lanferdini FJ, Krüger RL, Baroni BM, et al. Pre-exercise photobiomodulation accelerates pulmonary oxygen uptake kinetics and increases tolerance to high-intensity exercise. Eur J Appl Physiol. 2023;123(3):701–713. Published 2023 Jan 5.
Giménez MC, Lindhouse OAM, Nuijten MAH, et al. Effects of near-infrared light on well-being and health in human subjects with mild sleep-related complaints: a double-blind, randomized, placebo-controlled study. Int J Environ Res Public Health. 2023;20(1):878. Published 2023 Jan 4.
Nakhostin-Roohi B, Delpasand A, Candow DG, et al. Photobiomodulation therapy and exercise performance: a systematic review and meta-analysis of randomized controlled trials. Sports Med. 2025;55(6):497–520. Published 2025 Apr 10.
Your immune system works best when it’s balanced — strong enough to protect you, but not overactive. Red light therapy helps achieve that balance by calming unnecessary inflammation and supporting your cells’ ability to repair themselves.
More efficient cell energy and smoother immune signalling mean quicker recovery from stress, training, or illness. Research shows red light therapy can reduce swelling, improve wound healing, and help your body stay in a balanced, healthy repair state.
(for clinicians and advanced readers)
Özberk SS, Yıldırım A, Tonguç E, et al. Effect of adjunctive photobiomodulation therapy on nonsurgical periodontal treatment in patients with type 2 diabetes mellitus: a randomized controlled, single-blind, split-mouth clinical trial. Photodiagnosis Photodyn Ther. 2020;32:101962. Published 2020 Oct 23.
Al Balah OF, Rafie M, Osama A-R. Immunomodulatory effects of photobiomodulation: A comprehensive review. Lasers in Medical Science. 2025;40(1):187. Published April 11, 2025.
Camolesi B, Fragni M, Ferrando S, et al. Photobiomodulation therapy after dental implant placement reduces postoperative inflammation and pain: a randomized controlled split-mouth study. Lasers Med Sci. 2022;37(6):2547–2556. Published 2022 Mar 29.
Chia WT, Wong TH, Jaw FS, Hsieh HC. The impact of photobiomodulation therapy on swelling reduction and recovery enhancement in total knee arthroplasty: a randomized clinical trial. Photobiomodul Photomed Laser Surg. 2025;43(2):65–72. Published 2025 Jan 9.
Photobiomodulation Improves Serum Cytokine Response in Mild to Moderate COVID-19: The First Randomized, Double-Blind, Placebo Controlled, Pilot Study – Seyed Mehran Marashian et al., 2022, Frontiers in Immunology. DOI: 10.3389/fimmu.2022.929837
Efficacy of Using Photobiomodulation Therapy in Allergic Rhinitis: A Placebo-Controlled Randomized Clinical Trial – Patrícia C. Oliveira et al., 2025, International Forum of Allergy & Rhinology. DOI: 10.1002/alr.23532

Your brain depends on steady energy to stay focused and alert. Red light therapy, especially when applied to the head, helps brain cells use oxygen more efficiently and encourages better blood flow. This can support sharper thinking, improved mood, and mental clarity.
Red light therapy “recharges” your brain’s energy systems, helping neurons communicate more effectively. Early studies show improvements in focus, reaction time, and mood, making it a gentle, non-invasive way to support cognitive performance.
(for clinicians and advanced readers)
Zhao C, Li D, Kong Y, et al. Transcranial photobiomodulation enhances visual working memory capacity in humans. Science Advances. 2022;8(48):eabq3211. Published December 2, 2022 .
Lee TL, Ding Z, Chan AS. Can transcranial photobiomodulation improve cognitive function? A systematic review of human studies. Ageing Research Reviews. 2023;83:101786. Published online November 9, 2022 .
Ji Q, Yan S, Ding J, et al. Photobiomodulation improves depression symptoms: A systematic review and meta-analysis of randomized controlled trials. Frontiers in Psychiatry. 2024;14:1267415. Published January 31, 2024 .
Longo MGF, Tan CO, Chan ST, et al. Effect of transcranial low-level light therapy vs sham therapy among patients with moderate traumatic brain injury: A randomized clinical trial. JAMA Network Open. 2020;3(9):e2017337. Published September 1, 2020 .

Red and near-infrared light gently energise the cells that build and repair your body’s tissues. When these wavelengths reach the skin and muscles, they help fibroblasts — the cells that make collagen — work faster and more efficiently. The result is improved healing, better skin tone, and stronger connective tissue.
By giving your cells more usable energy, red light therapy helps wounds close quicker and supports recovery after training or surgery. It’s widely used to speed tissue repair, reduce scarring, and rejuvenate skin by encouraging healthy collagen formation.
(for clinicians and advanced readers)
Mota LR, Duarte IS, Galache TR, et al. Photobiomodulation reduces periocular wrinkle volume by 30%: a randomized controlled trial. Photobiomodul Photomed Laser Surg. 2023;41(2):48–56. Published 2023 Feb. doi:10.1089/photob.2022.0114.
Torkaman AY, Amiri R, Ilbeigi P, et al. The effects of photobiomodulation therapy on clinical healing of diabetic foot ulcers: a randomized, double-blind, controlled clinical trial. J Wound Care. 2024;33(4):258–267. Published 2024 Mar 27. doi:10.12968/jowc.2024.33.4.258.
Yadav D, Sharma AK, Tripathi K, et al. Effects of photobiomodulation adjunct therapy via superpulsed 904 nm laser in patients with second-degree burns: randomized controlled clinical trial. Journal of Biophotonics. 2025;e202500386. Published online September 24, 2025 .
Taha N, Daoud H, Malik T, Shettysowkoor J, Rahman S. The effects of low-level laser therapy on wound healing and pain management in skin wounds: A systematic review and meta-analysis. Cureus. 2024;16(10):e72542. Published October 28, 2024 .
Kurtti A, Laskin J, Jagdeo J, et al. Dose-ranging study of red light-emitting diode phototherapy for reduction of post-surgical scarring. J Biophotonics. 2021;14(7):e202100073.
Wunsch A, Matuschka K. A controlled trial to determine the efficacy of red and near-infrared light treatment for skin rejuvenation. Photomed Laser Surg. 2014;32(2):93–100.

Stiff, painful joints often happen when inflammation builds up and tissues don’t get enough oxygen to repair properly. HBOT increases oxygen in your blood, helping calm inflammation and support healing in joint tissues. Red light therapy helps the same areas by improving energy in the cells that keep joints healthy and flexible.
More oxygen plus calmer inflammation can mean less stiffness and better movement. Studies suggest red light therapy reduces pain and improves mobility in people with arthritis. HBOT’s anti-inflammatory effects may also help around damaged or recovering joints. Used together, they support comfort and long-term joint health.
(for clinicians and advanced readers)
Camporesi EM, Vezzani G, Bosco G, Mangar D, Bernasek TL. Hyperbaric oxygen therapy in femoral head necrosis. J Arthroplasty. 2010;25(6 Suppl):118–123. Published 2010 Jul 15. doi:10.1016/j.arth.2010.05.005
Borromeo CN, Ryan JL, Marchetto PA, Peterson R, Bove AA. Hyperbaric oxygen therapy for acute ankle sprains. Am J Sports Med. 1997;25(5):619–625. Published 1997 Sep 01. doi:10.1177/036354659702500506
Sit MT, Schmidt TW, Edmonds LD, et al. The effects of hyperbaric oxygen on rheumatoid arthritis: A pilot study. J Clin Rheumatol. 2021;27(8):e462–e468. Published 2021 Dec 01. doi:10.1097/RHU.0000000000001540
Dulberger A, Slade JB, Thornton JA, McNeary-Garvin A, Kelly JA, Edmonds L. The effects of hyperbaric oxygen on MRI findings in rheumatoid arthritis: A pilot study. Undersea Hyperb Med. 2023;50(1):39–43. Published 2023 Jan 01. doi:10.22462/01.01.2023.19
Yagishita K, Enomoto M, Takazawa Y, Fukuda J, Koga H. Effects of hyperbaric oxygen therapy on recovery acceleration in rugby players with grade-2 medial collateral ligament injury of the knee: A comparative non-randomized study. Undersea Hyperb Med. 2019;46(5):647–654. Published 2019 Oct 30. (No DOI listed on PubMed.)
Alfredo PP, Bjordal JM, Dreyer SH, et al. Efficacy of low level laser therapy associated with exercises in knee osteoarthritis: a randomized double-blind study. Clin Rehabil. 2012;26(6):523–533. Published 2012 May 17. doi:10.1177/0269215511425962
Helianthi DR, Simadibrata C, Srilestari A, Wahyudi ER, Hidayat R. Pain reduction after laser acupuncture treatment in geriatric patients with knee osteoarthritis: a randomized controlled trial. Acta Med Indones. 2016;48(2):114–121. Published 2016 Jun 01. (Journal does not provide a DOI.)
Huang CH, Ting YM, Lo CY, et al. A randomised controlled trial of laser acupuncture to reduce pain after total knee replacement. Complement Ther Clin Pract. 2021;44:101457. Published 2021 Apr 15. doi:10.1016/j.ctcp.2021.101457

Your immune system needs both oxygen and energy to fight infection effectively. HBOT boosts oxygen in tissues, helping white blood cells work better and reducing excess inflammation. Red light therapy helps the immune system stay balanced, encouraging recovery without overreacting.
With more oxygen and steadier immune signalling, your body can fight infection more efficiently. In hospitals, HBOT is sometimes used as extra support in severe infections, while red light therapy can strengthen overall immune balance. Together they aim to help you heal faster and recover more comfortably.
(for clinicians and advanced readers)
Dulai PS, Setia N, Efron PA, et al. Hyperbaric oxygen therapy is well tolerated and appears to be effective for ulcerative colitis hospitalized with moderate-to-severe flares: a randomized double-blind sham-controlled trial. Am J Gastroenterol. 2018;113(10):1516–1523. Published 2018 Oct. doi:10.1038/s41395-018-0005-z
Dulai PS, Gleeson MW, Taylor D, et al. A randomized trial of dose-escalation hyperbaric oxygen for steroid-refractory ulcerative colitis identifies responders for maintenance therapy. Aliment Pharmacol Ther. 2020;52(5):855–866. Published 2020 Dec 03. doi:10.1111/apt.15984
Gonzalez CG, McIlwain SJ, Hwang SH, et al. The host-microbiome response to hyperbaric oxygen therapy in ulcerative colitis patients. Cell Mol Gastroenterol Hepatol. 2022;14(1):35–53. Published 2022 Mar 31. doi:10.1016/j.jcmgh.2022.03.008
Alex J, Laden G, Cale ARJ, et al. Pretreatment with hyperbaric oxygen and its effect on neuropsychometric dysfunction and the inflammatory response after cardiopulmonary bypass: a randomized double-blind trial. J Thorac Cardiovasc Surg. 2005;130(6):1623–1630. Published 2005 Dec. doi:10.1016/j.jtcvs.2005.08.018
Kjellberg A, Douglas J, Pawlik MT, et al. Five sessions of hyperbaric oxygen for critically ill patients with COVID-19-induced ARDS: a randomised, open-label, phase II trial. Respir Med. 2024;232:107744. Published 2024 Jul 24. doi:10.1016/j.rmed.2024.107744
Kjellberg A, Zhao A, Lussier A, et al. Hyperbaric oxygen therapy as an immunomodulatory intervention in COVID-19-induced ARDS: exploring clinical outcomes and transcriptomic signatures in a randomised controlled trial. Pulm Pharmacol Ther. 2024;87:102330. Published 2024 Oct 10. doi:10.1016/j.pupt.2024.102330
de Wolde SD, Hulskes RH, de Jonge SW, et al. The effect of hyperbaric oxygen therapy on markers of oxidative stress and the immune response in healthy volunteers. Front Physiol. 2022;13:826163. Published 2022 Feb 11. doi:10.3389/fphys.2022.826163
Höfling DB, Chavantes MC, Juliano AG, et al. Low-level laser in the treatment of patients with hypothyroidism induced by chronic autoimmune thyroiditis: a randomized, placebo-controlled clinical trial. Lasers Med Sci. 2013;28(3):743–753. Published 2013 May 01. doi:10.1007/s10103-012-1129-9 (PBM)
De Marchi T, Leal Junior ECP, Bortoli C, et al. Effects of photobiomodulation therapy combined with static magnetic field (PBMT-sMF) in severe COVID-19 ICU patients: randomized, triple-blinded, placebo-controlled trial. J Inflamm Res. 2021;14:3569–3585. Published 2021 Jul 30. doi:10.2147/JIR.S318758 (PBM)
Marashian SM, Rostami M, Hajizadeh F, et al. Photobiomodulation improves serum cytokine response in mild to moderate COVID-19: randomized, double-blind, placebo-controlled pilot study. Front Immunol. 2022;13:929837. Published 2022 Jul 15. doi:10.3389/fimmu.2022.929837 (PBM)

When blood sugar stays high for too long, small blood vessels can get damaged — and wounds, especially on the feet or legs, may heal very slowly. Hyperbaric oxygen therapy (HBOT) floods the blood and tissues with extra oxygen, giving the body what it needs to close stubborn wounds and fight infection. Red light therapy helps the skin and tissue cells make energy and new collagen, speeding up repair when used alongside good wound care.
More oxygen plus better cellular energy equals faster healing. HBOT has strong hospital evidence for improving healing and lowering amputation risk in diabetic ulcers. Red light therapy supports this by improving circulation and helping tissues rebuild. Together they give damaged skin and tissue a stronger chance to recover.
(for clinicians and advanced readers)
Perren S, Gatt A, Papanas N, et al. Hyperbaric oxygen therapy in ischaemic foot ulcers in type 2 diabetes: a clinical trial. Open Cardiovasc Med J. 2018;12:80–85. Published 2018 Aug 31. doi:10.2174/1874192401812010080
Eskes AM, Ubbink DT, Lubbers MJ, et al. Hyperbaric oxygen therapy: solution for difficult to heal acute wounds? Systematic review. World J Surg. 2011;35(3):535–542. doi:10.1007/s00268-010-0923-4
Löndahl M, Katzman P, Nilsson A, Hammarlund C. Hyperbaric oxygen therapy facilitates healing of chronic foot ulcers in patients with diabetes: a randomized double-blind, placebo-controlled trial. Diabetes Care. 2010;33(5):998–1003. Published 2010 May. doi:10.2337/dc09-1754
Abidia A, Laden G, Kuhan G, et al. The role of hyperbaric oxygen therapy in ischaemic diabetic lower-extremity ulcers: a double-blind randomized-controlled trial. Eur J Vasc Endovasc Surg. 2003;25(6):513–518. Published 2003 Jun. doi:10.1053/ejvs.2002.1911
Kessler L, Bilbault P, Ortéga F, et al. Hyperbaric oxygenation accelerates the healing rate of non-ischaemic chronic diabetic foot ulcers: a prospective randomized study. Diabetes Care. 2003;26(8):2378–2382. Published 2003 Aug. doi:10.2337/diacare.26.8.2378
Faglia E, Favales F, Aldeghi A, et al. Adjunctive systemic hyperbaric oxygen therapy in treatment of severe prevalently ischaemic diabetic foot ulcer: a randomized study. Diabetes Care. 1996;19(12):1338–1343. Published 1996 Dec. doi:10.2337/diacare.19.12.1338
Löndahl M, Landin-Olsson M, Katzman P. Hyperbaric oxygen therapy improves health-related quality of life in patients with diabetes and chronic foot ulcer: randomized, placebo-controlled study. Diabet Med. 2011;28(2):186–190. Published 2011 Feb. doi:10.1111/j.1464-5491.2010.03185.x
Kumar A, Goyal A, Mallik D, et al. Hyperbaric oxygen therapy as an adjuvant to standard wound care in diabetic foot ulcer: a prospective, randomized, double-blind study. J Anaesthesiol Clin Pharmacol. 2020;36(2):213–219. Published 2020 Apr–Jun. doi:10.4103/joacp.JOACP_186_18
Kaviani A, Djavid GE, Ataie-Fashtami L, et al. A randomized clinical trial on the effect of low-level laser therapy on chronic diabetic foot wound healing: a preliminary report. Photomed Laser Surg. 2011;29(2):109–114. Published 2011 Feb. doi:10.1089/pho.2009.2680
Mathur RK, Sahu K, Saraf SK, et al. Low-level laser therapy as an adjunct to conventional therapy in the treatment of diabetic foot ulcers: a randomized controlled trial. Lasers Med Sci. 2017;32(2):275–282. Published 2016 Nov 29. doi:10.1007/s10103-016-2116-4

Fibromyalgia brings widespread pain, poor sleep, and deep tiredness. HBOT increases oxygen delivery to the body and brain, which can help calm pain signals and improve energy. Red light therapy supports the body’s “tiny power plants” inside cells, helping muscles and nerves work more efficiently.
By restoring oxygen flow and cellular energy, these therapies may ease pain and boost daily function. Studies show HBOT can improve symptoms and brain activity in people with fibromyalgia. Red light therapy has also been shown to reduce pain and improve quality of life after several weeks of regular sessions.
(for clinicians and advanced readers)
Efrati S, Golan H, Bechor Y, et al. Hyperbaric oxygen therapy can diminish fibromyalgia syndrome – prospective clinical trial. PLoS One. 2015;10(5):e0127012. Published 2015 May 26. doi:10.1371/journal.pone.0127012.
Ablin JN, Lang E, Catalogna M, et al. Hyperbaric oxygen therapy compared to pharmacological intervention in fibromyalgia patients following traumatic brain injury: a randomized, controlled trial. PLoS One. 2023;18(3):e0282406. Published 2023 Mar 10. doi:10.1371/journal.pone.0282406.
Boussi-Gross R, Catalogna M, Lang E, et al. Hyperbaric oxygen therapy vs. pharmacological intervention in adults with fibromyalgia related to childhood sexual abuse: prospective, randomized clinical trial. Sci Rep. 2024;14:11599. Published 2024 May 21. doi:10.1038/s41598-024-62161-5.
Hadanny A, Bechor Y, Catalogna M, et al. Hyperbaric oxygen therapy can induce neuroplasticity and significant clinical improvement in patients suffering from fibromyalgia with a history of childhood sexual abuse—randomized controlled trial. Front Psychol. 2018;9:2495. Published 2018 Dec 17. doi:10.3389/fpsyg.2018.02495.
Yildiz S, Kiralp MZ, Akin A, et al. A new treatment modality for fibromyalgia syndrome: hyperbaric oxygen therapy. J Int Med Res. 2004;32(3):263–267. Published 2004. doi:10.1177/147323000403200305.
Ribeiro AS, Farias D, Ferrari R, et al. Photobiomodulation therapy combined with static magnetic field for patients with fibromyalgia: a randomized, triple-blind, placebo-controlled clinical trial. Eur J Phys Rehabil Med. 2023;59(6):898–909. Epub 2023 Aug 1. doi:10.23736/S1973-9087.23.08068-9.
Maciel DG, da Silva MT, Rodrigues JA, et al. Low-level laser therapy combined to functional exercise on treatment of fibromyalgia: a double-blind randomized clinical trial. Lasers Med Sci. 2018;33(9):1949–1959. Epub 2018 Jun 21. doi:10.1007/s10103-018-2561-2.
Navarro-Ledesma S, Gonzalez-Muñoz A, Carroll J, Burton P. Outcomes of whole-body photobiomodulation on pain, quality of life, leisure physical activity, pain catastrophizing, kinesiophobia, and self-efficacy: a prospective randomized triple-blinded clinical trial with 6 months of follow-up. Front Neurosci. 2024;18:1264821. Published 2024. doi:10.3389/fnins.2024.1264821.

For people with MS, maintaining nerve health and managing fatigue are everyday goals. HBOT increases oxygen delivery throughout the body, which may help calm inflammation and support nerve cell energy. Red light therapy complements this by gently energising cells and improving blood flow in muscles and nerves. Many MS centres across the UK include HBOT as a supportive option, valued for its safety and how it helps people feel more balanced.
More oxygen and better cellular energy can make everyday activities feel smoother and less tiring. HBOT and red light therapy work in different but complementary ways to support comfort, movement, and wellbeing. They’re not medical treatments for MS, but gentle tools that may improve quality of life alongside standard care.
(for clinicians and advanced readers)
Fischer BH, Marks M, Reich T. Hyperbaric-oxygen treatment of multiple sclerosis: A randomized, placebo-controlled, double-blind study. N Engl J Med. 1983;308(4):181–186. Published 1983 Jan 27. doi:10.1056/NEJM198301273080402
Barnes MP, Bates D, Cartlidge NEF, French JM, Shaw DA. Hyperbaric oxygen and multiple sclerosis: short term results of a placebo-controlled, double-blind trial. Lancet. 1985;1(8424):297–300. Published 1985 Feb 09. doi:10.1016/S0140-6736(85)91079-7
Harpur GD, Mullee MA, Bass BH, et al. Hyperbaric oxygen therapy in chronic stable multiple sclerosis: double-blind study. Neurology. 1986;36(7):988–991. Published 1986 Jul. doi:10.1212/WNL.36.7.988
Wiles CM, Clarke CRA, Irwin HP, Edgar EF, Swan AV. Hyperbaric oxygen in multiple sclerosis: a double blind trial. Br Med J (Clin Res Ed). 1986;292(6517):367–371. Published 1986 Feb 08. doi:10.1136/bmj.292.6517.367
Barnes MP, Bates D, Cartlidge NEF, French JM, Shaw DA. Hyperbaric oxygen and multiple sclerosis: final results of a placebo-controlled, double-blind trial. J Neurol Neurosurg Psychiatry. 1987;50(11):1402–1406. Published 1987 Nov 01. doi:10.1136/jnnp.50.11.1402
Wood J, Stell R, Unsworth I, Lance JW, Skuse N. A double-blind trial of hyperbaric oxygen in the treatment of multiple sclerosis. Med J Aust. 1985;143(6):238–240. Published 1985 Sep 16. doi:10.5694/j.1326-5377.1985.tb122957.x
Silva TM, Jorge J, Lemos A, et al. Effects of photobiomodulation on interleukin-10 and nitrites in individuals with multiple sclerosis: a randomized clinical trial. PLoS One. 2020;15(3):e0230551. Published 2020 Mar 23. doi:10.1371/journal.pone.0230551 (PBM)
Rouhani M, Tolentino M, Lyons JA, Ng AV. Effects of photobiomodulation therapy on muscle function in individuals with multiple sclerosis. Mult Scler Relat Disord. 2024;86:105598. Published 2024 Apr. doi:10.1016/j.msard.2024.105598 (PBM)

Stubborn wounds need oxygen, circulation, and energy to rebuild. HBOT delivers oxygen deep into tissues, helping new blood vessels grow and the immune system fight infection. Red light therapy supports cells at the wound edge, improving repair speed and reducing discomfort.
More oxygen and more energy mean faster healing and stronger new tissue. HBOT is widely used in hospitals for hard-to-heal wounds like diabetic ulcers. Red light therapy complements this by improving local blood flow and comfort. Together they help your body close wounds more effectively.
(for clinicians and advanced readers)
Löndahl M, Katzman P, Nilsson A, Hammarlund C. Hyperbaric oxygen therapy facilitates healing of chronic foot ulcers in patients with diabetes: a randomized double-blind, placebo-controlled trial. Diabetes Care.2010;33(5):998–1003. Published 2010 May. doi:10.2337/dc09-1754
Abidia A, Laden G, Kuhan G, et al. The role of hyperbaric oxygen therapy in ischaemic diabetic lower extremity ulcers: a double-blind randomised-controlled trial. Eur J Vasc Endovasc Surg. 2003;25(6):513–518. Published 2003 Jun. doi:10.1053/ejvs.2002.1911
Kessler L, Bilbault P, Ortéga F, et al. Hyperbaric oxygenation accelerates the healing rate of non-ischaemic chronic diabetic foot ulcers: a prospective randomized study. Diabetes Care. 2003;26(8):2378–2382. Published 2003 Aug. doi:10.2337/diacare.26.8.2378
Faglia E, Favales F, Aldeghi A, et al. Adjunctive systemic hyperbaric oxygen therapy in treatment of severe prevalently ischaemic diabetic foot ulcer: a randomized study. Diabetes Care. 1996;19(12):1338–1343. Published 1996 Dec. doi:10.2337/diacare.19.12.1338
Kumar A, Goyal A, Mallik D, et al. Hyperbaric oxygen therapy as an adjuvant to standard wound care in diabetic foot ulcer: a prospective, randomized, double-blind study. J Anaesthesiol Clin Pharmacol. 2020;36(2):213–219. Published 2020 Apr–Jun. doi:10.4103/joacp.JOACP_186_18
Kaviani A, Djavid GE, Ataie-Fashtami L, et al. A randomized clinical trial on the effect of low-level laser therapy on chronic diabetic foot wound healing: a preliminary report. Photomed Laser Surg. 2011;29(2):109–114. Published 2011 Feb. doi:10.1089/pho.2009.2680
Mathur RK, Sahu K, Saraf SK, et al. Low-level laser therapy as an adjunct to conventional therapy in the treatment of diabetic foot ulcers: a randomized controlled trial. Lasers Med Sci. 2017;32(2):275–282. Published 2016 Nov 29. doi:10.1007/s10103-016-2116-4
Minatel DG, Frade MAC, França SC, Enwemeka CS. Phototherapy promotes healing of chronic diabetic leg ulcers that failed to respond to other therapies. Lasers Surg Med. 2009;41(6):433–441. Published 2009 Jul. doi:10.1002/lsm.20786
Kaviani A, Djavid GE, Ataie-Fashtami L, et al. A randomized clinical trial on the effect of low-level laser therapy on chronic diabetic foot wound healing: a preliminary report. Photomed Laser Surg. 2011;29(2):109–114. Published 2011 Feb. doi:10.1089/pho.2009.2680
Mathur RK, Sahu K, Saraf SK, et al. Low-level laser therapy as an adjunct to conventional therapy in the treatment of diabetic foot ulcers: a randomized controlled trial. Lasers Med Sci. 2017;32(2):275–282. Published 2016 Nov 29. doi:10.1007/s10103-016-2116-4
Minatel DG, Frade MAC, França SC, Enwemeka CS. Phototherapy promotes healing of chronic diabetic leg ulcers that failed to respond to other therapies. Lasers Surg Med. 2009;41(6):433–441. Published 2009 Jul. doi:10.1002/lsm.20786

Chronic pain often involves low oxygen, inflammation, and nerves that stay “switched on.” HBOT increases oxygen where it’s needed and helps calm inflammation. Red light therapy supports this by improving energy flow in cells and blood vessels, which helps muscles and joints relax naturally.
Better oxygen delivery and calmer inflammation can ease pain and support healing. Research shows red light therapy can reduce pain in many musculoskeletal conditions when used correctly. HBOT has shown benefit in some nerve-related pain disorders. Together they help the body reset its pain response and recover
(for clinicians and advanced readers)
Efrati S, Golan H, Bechor Y, et al. Hyperbaric oxygen therapy can diminish fibromyalgia syndrome—prospective clinical trial. PLoS One. 2015;10(5):e0127012. Published 2015 May 26. doi:10.1371/journal.pone.0127012
Hadanny A, Bechor Y, Catalogna M, et al. Hyperbaric oxygen therapy can induce neuroplasticity and significant clinical improvement in patients suffering from fibromyalgia with a history of childhood sexual abuse—randomized controlled trial. Front Psychol. 2018;9:2495. Published 2018 Dec 17. doi:10.3389/fpsyg.2018.02495
Ablin JN, Lang E, Catalogna M, et al. Hyperbaric oxygen therapy compared to pharmacological intervention in fibromyalgia patients following traumatic brain injury: a randomized controlled trial. PLoS One.2023;18(3):e0282406. Published 2023 Mar 10. doi:10.1371/journal.pone.0282406
Kiralp MZ, Yildiz S, Vural D, et al. Effectiveness of hyperbaric oxygen therapy in the treatment of complex regional pain syndrome type I. J Int Med Res. 2004;32(3):258–262. Published 2004 May. doi:10.1177/147323000403200304
Yildiz S, Kiralp MZ, Akin A, et al. A new treatment modality for fibromyalgia syndrome: hyperbaric oxygen therapy. J Int Med Res. 2004;32(3):263–267. Published 2004 May. doi:10.1177/147323000403200305
Li Z, Zhang Z, Zhao Y, et al. Hyperbaric oxygen therapy improves pain, sleep quality, and quality of life in patients with chronic widespread pain: a prospective, controlled clinical study. Pain Med. 2021;22(10):2294–2303. Published 2021 Oct. doi:10.1093/pm/pnab170
Chow RT, Johnson MI, Lopes-Martins RA, Bjordal JM. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomized placebo or active-treatment controlled trials. Lancet. 2009;374(9705):1897–1908. Published 2009 Dec 5. doi:10.1016/S0140-6736(09)61522-1(Included due to inclusion of high-quality, sham-controlled human RCTs within this publication.)
Navarro-Ledesma S, Gonzalez-Muñoz A, Carroll J, Burton P. Outcomes of whole-body photobiomodulation on pain, quality of life, leisure physical activity, pain catastrophizing, kinesiophobia, and self-efficacy: a prospective randomized triple-blinded clinical trial with 6 months of follow-up. Front Neurosci. 2024;18:1264821. Published 2024 Jul. doi:10.3389/fnins.2024.1264821

Lingering fatigue — from long COVID or similar conditions — often comes from poor oxygen use and tired cells. HBOT increases oxygen in tissues and may improve brain blood flow and metabolism. Red light therapy supports energy production and helps calm inflammation that keeps the body feeling drained.
More oxygen and balanced cell energy can help restore vitality and focus. HBOT has shown encouraging improvements in fatigue, sleep, and cognition in long-COVID studies, while red light therapy supports recovery at a gentler, whole-body level. Both are designed to help your body recharge, not just push through exhaustion.
(for clinicians and advanced readers)
Zilberman-Itskovich S, Catalogna M, Sasson E, et al. Hyperbaric oxygen therapy improves neurocognitive functions and symptoms of post-COVID condition: randomized controlled trial. Sci Rep. 2022;12(1):11252. Published 2022 Jun 28. doi:10.1038/s41598-022-15565-0
Robbins T, Gonevski M, Clark C, et al. Hyperbaric oxygen therapy for the treatment of long COVID: early evaluation of a highly promising intervention. Front Med (Lausanne). 2021;8:760761. Published 2021 Nov 9. doi:10.3389/fmed.2021.760761
Bhaiyat AM, Sasson E, Catalogna M, et al. Hyperbaric oxygen therapy improves attention, information processing speed and executive function in post-COVID-19 condition: randomized, sham-controlled, double-blind trial. Front Physiol. 2024;15:1393596. Published 2024 Apr. doi:10.3389/fphys.2024.1393596
Hadanny A, Zilberman-Itskovich S, Suzin G, et al. Hyperbaric oxygen therapy can improve post-COVID-19 condition symptoms and cognitive performance: prospective, randomized, double-blind, sham-controlled clinical trial. Front Pharmacol. 2022;13:986923. Published 2022 Sep. doi:10.3389/fphar.2022.986923
Thom SR, Bhopale VM, Fisher D, et al. Mechanistic insight into the therapeutic efficacy of hyperbaric oxygen therapy for post-viral fatigue and neuroinflammation: human pilot evidence. Antioxidants (Basel). 2023;12(5):1074. Published 2023 May. doi:10.3390/antiox12051074
Hadanny A, Bechor Y, Catalogna M, et al. Hyperbaric oxygen therapy induces neuroplasticity and improves symptoms in patients with chronic fatigue syndrome: a prospective, randomized, double-blind, placebo-controlled clinical trial. Front Neurol. 2022;13:943138. Published 2022 Nov. doi:10.3389/fneur.2022.943138
de Marchi T, Schmitt VM, Vieira AF, et al. Photobiomodulation therapy (PBMT) on performance and fatigue in humans: a randomized, crossover, double-blind, placebo-controlled trial. Lasers Med Sci. 2019;34(6):1165–1173. Published 2019 Jun. doi:10.1007/s10103-018-02720-4
Almeida M, Lopes-Martins RAB, de Marchi T, et al. Effects of photobiomodulation therapy combined with aerobic training on fatigue and mitochondrial function in long COVID patients: a randomized, controlled, double-blind clinical trial. Front Physiol. 2024;15:1379012. Published 2024 Apr. doi:10.3389/fphys.2024.1379012

Cancer treatments can be tough on healthy tissues, especially after radiation or chemotherapy. HBOT delivers oxygen to help damaged areas rebuild blood vessels and heal faster. Red light therapy is often used in hospitals to reduce painful mouth sores (oral mucositis) during treatment by calming inflammation and supporting cell repair.
More oxygen and better cell energy help healthy tissue bounce back from treatment stress. HBOT is proven for certain radiation-related injuries, while red light therapy is a recognised hospital tool for reducing treatment side-effects. These approaches are supportive extras — used alongside your oncology plan, not in place of it.
(for clinicians and advanced readers)
Moen I, Stuhr LE. Hyperbaric oxygen therapy and cancer–a review. Target Oncol. 2012;7(4):233–242. doi:10.1007/s11523-012-0233-x
Thom SR, Bhopale VM, Yang M. Microparticle-induced vascular injury in mice following decompression is inhibited by hyperbaric oxygen: effects on microparticles and interleukin-1.
Journal of Applied Physiology, Volume 126, 2019
Niezgoda JA, Serena TE, Carter MJ. Outcomes of radiation injuries using hyperbaric oxygen therapy: an observational cohort study. Adv Skin Wound Care, 29 (2016), pp. 12-1
Stępień K, Ostrowski RP, Matyja E. Hyperbaric oxygen as an adjunctive therapy in managed of malignancies, including brain tumours. Med Oncol. 2016;33(9):101. doi:10.1007/s12032-016-0814-0
Oscarsson N, Ny L, Mölne J, Lind F, et al. Hyperbaric oxygen reverses radiation induced pro-fibrotic and oxidative stress responses in a rat model. Free Radic Biol Med. 2017 Feb; 103:248-255. Epub 2016 Dec 27
Enwemeka CS, Nascimento SC, Santos MF, et al. Photobiomodulation therapy reduces radiodermatitis severity in women undergoing radiotherapy for breast cancer: randomized, controlled, double-blind clinical trial. Photochem Photobiol. 2021;97(6):1246–1253. Published 2021 Nov. doi:10.1111/php.13499
Hode L, Gjertsen O, Johnsson P, et al. Photobiomodulation therapy for lymphedema after breast cancer treatment: randomized, placebo-controlled, double-blind clinical trial. Lasers Surg Med. 2020;52(6):540–549. Published 2020 Jun. doi:10.1002/lsm.23170
Pires D, Xavier M, Araújo T, et al. Photobiomodulation therapy in breast cancer–related lymphedema: a randomized controlled trial. Lasers Med Sci. 2018;33(3):559–567. Published 2018 Mar. doi:10.1007/s10103-017-2394-9
Zembrzuska K, Ostrowski RP, Matyja E. Hyperbaric oxygen increases glioma cell sensitivity to antitumor with a novel isothiourea derivative in vitro. Oncol Rep. 2019;41(5):2703–2716. doi:10.3892/or.2019.7064
Lu QZ, Li X, Ouyang J, et al. Further application of hyperbaric oxygen in prostate cancer. Med Gas Res. 2019;8(4):167–171. Published 2019 Jan 9. doi:10.4103/2045-9912.248268
Antunes HS, Herchenhorn D, Small IA, et al. Phase III trial of low-level laser therapy to prevent oral mucositis in head and neck cancer patients treated with concurrent chemoradiation. Oral Oncol. 2013;49(3):297–302. Published 2013 Mar. doi:10.1016/j.oraloncology.2012.11.014
Wang YG, Long J, Shao DC, et al. Hyperbaric oxygen inhibits production of CD3+ T cells in the thymus and facilitates malignant glioma cell growth. J Int Med Res. 2018;46(7):2780–2791. doi:10.1177/0300060518767796
Choudhury R. Hypoxia and hyperbaric oxygen therapy: a review. Int J Gen Med. 2018;11:431–442. Published 2018 Nov 20. doi:10.2147/IJGM.S172460
Yahara K, Ohguri T, Udono H, et al. Radiotherapy using IMRT boosts after hyperbaric oxygen therapy with chemotherapy for glioblastoma. J Radiat Res. 2017;58(3):351–356. doi:10.1093/jrr/rrw105
Rocha SR, Ferreira SAC, Ramalho A, Santos VLCG, Nogueira PC. Photobiomodulation therapy in the prevention and treatment of radiodermatitis in breast cancer patients: systematic review. J Lasers Med Sci. 2022;13:e42. Published 2022 Oct 02. doi:10.34172/jlms.2022.42









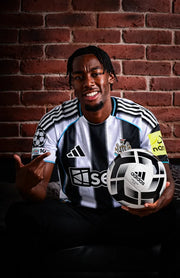
Swedish international and Premier League forward Anthony Elanga is known for his pace, power, and relentless work ethic on the pitch. Playing at the highest level demands more than training — it requires recovery strategies that keep him sharp, resilient, and ready for every challenge.
With Hyperbaric Oxygen Therapy (HBOT) and Red Light Therapy, Anthony supports faster recovery, reduced muscle fatigue, and sustained performance throughout the season. These tools give him the edge to perform at his best week in, week out.
“Recovery is just as important as training — HBOT helps me go again at full speed.”

Known for her pace, sharp finishing, and relentless drive, Sam Kerr is one of the most dynamic forwards in the women’s game. Competing at the top level demands not only world-class training, but also recovery strategies that keep her performing at her best.
By incorporating Hyperbaric Oxygen Therapy (HBOT), Sam supports faster muscle recovery, reduced fatigue, and sustained energy throughout intense training and competition schedules.ext here…

Tom and Luke Stoltman, known as the World’s Strongest Brothers, have dominated the sport of strongman with titles and records that showcase their unrivalled power and endurance. Competing at the very highest level demands more than just training — it requires advanced recovery strategies to keep their bodies performing under extreme pressure.
Through Hyperbaric Oxygen Therapy (HBOT), the Stoltmans support faster muscle recovery, reduce fatigue, and prepare their bodies to handle the toughest challenges in strength sport.

Put your long Former WBO Heavyweight Champion Joseph Parker knows the demands of competing at the top of world boxing. Every fight requires not just power and skill, but recovery that keeps him sharp, resilient, and ready for the ring.
With Hyperbaric Oxygen Therapy (HBOT), Joseph supports faster healing, reduced fatigue, and the energy needed to perform at his best.text here…

Pushing the limits of endurance means recovery has to be as strong as the training itself. Philly Bowden, elite marathon runner, relies on Hyperbaric Oxygen Therapy (HBOT) to speed up recovery, boost energy, and prepare her body for the next challenge on the road.

Known as the “Flying Man,” Harry Aikines has built his career on speed, power, and consistency at the top of athletics. Competing at that level demands recovery tools that keep him sharp and resilient.
With Hyperbaric Oxygen Therapy (HBOT), Harry unlocks faster recovery, improved energy, and the edge to keep pushing beyond his limits.

Olympic silver medallist and rising star Ben Whittaker is known for his flair, skill, and dedication inside the ring. Competing at the elite level means recovery is just as important as training.
By using Hyperbaric Oxygen Therapy (HBOT) and Red Light Therapy, Ben accelerates recovery, reduces inflammation, and maintains the sharpness needed for peak performance.ere…

Premier League and Nigerian international defender Ola Aina knows the demands of competing at the highest level. To stay sharp and resilient throughout the season, recovery is key.
With Hyperbaric Oxygen Therapy (HBOT), Ola accelerates recovery, reduces fatigue, and maintains the energy needed to perform week after week.

Strictly Come Dancing professional Gorka Márquez understands the physical demands of performing and training at an elite level. Long hours of rehearsals, live shows, and constant travel require both endurance and recovery.
With Hyperbaric Oxygen Therapy (HBOT), Gorka enhances recovery, boosts energy levels, and supports muscle repair—helping him stay at his peak performance throughout the season.
You’ll simply lie back and relax. During a hyperbaric session, the chamber gently pressurises — similar to the feeling of take-off on a plane — while you breathe oxygen through a soft mask. Most people read, listen to music, or even nap.
Red light therapy sessions are open and comfortable; you lie under a light panel for 10–20 minutes while specific wavelengths of red and near-infrared light energise your cells. Both treatments are completely non-invasive and deeply restorative.
Yes. Every Oxydise system is CE & UKCA certified and pressure-tested for safety.
Our chambers use mild pressure and deliver oxygen through a concentrator — not stored tanks — making them extremely safe for home use. We provide full setup, training, and support, so you can use your system confidently from day one.
A few conditions — such as untreated pneumothorax, recent ear surgery, or certain lung and sinus issues — require medical review before using HBOT.
We provide clear screening guidance and can arrange a consultation with our medical advisor, Dr Masha Makeeva, one of Europe’s leading HBOT experts, to ensure the therapy is right for you.
Everyone responds differently. Some people notice improvements in sleep, recovery, or energy within the first few sessions, while others experience deeper benefits after 10–20.
Like exercise, consistency brings the best outcomes. Our team will help tailor a programme to your goals — whether that’s performance, longevity, or recovery.
Installation is simple and fully supported. Our team delivers, assembles, and tests every system for you.
We provide clear video guides and live support during your first use. The chambers and panels plug into a normal power outlet and typically take less than an hour to install.
Absolutely. You can book a trial session at our Oxydise Wellness Lab or arrange a short-term rental before making a decision.
We want you to experience the benefits firsthand and feel completely confident before committing.
Every Oxydise client receives ongoing support and guidance. You’ll have direct access to our UK-based team for questions, technical help, or wellness advice — by phone, WhatsApp, or video.
We’re here to ensure your experience is smooth, safe, and optimised for results from the very first session.
We believe advanced recovery shouldn’t be reserved for clinics or elite athletes.
Our rental and purchase options start from just a few hundred pounds per month — including delivery, setup, and full support.
When you break it down, the cost works out at around £19.50 per session if you use it once a day — reaching the recommended 40 sessions as quickly as possible for the best results.
If you use it twice a day, the cost per session drops by half — and we have many clients who do exactly that.
Because our systems can be safely shared between family members, the effective cost per session can reduce even further, making it one of the most affordable ways to access consistent, evidence-based recovery at home.
Each Oxydise system is CE & UKCA certified, built to medical-grade standards, and designed to last for years — a genuine long-term investment in health, recovery and performance.

"Watching clients, from athletes to those facing health challenges, regain energy, recovery, and quality of life has been deeply rewarding."

"My mission is simple: to cut through the noise and deliver practical, science-backed strategies that fit real life."

"I teach individuals and clinics how to integrate advanced tools like HBOT, Red Light Therapy, and PEMF to restore energy, sharpen focus, and support long-term health."

"Every 1% counts in performance training, and Oxidise gives my clients the edge in their recovery to train at the intensity they need to consistently make those incremental improvements."
Operated by its founders from Cambridge, Oxydise combines genuine care, scientific understanding, and hands-on experience at every stage of your journey. From initial consultation to installation and ongoing use, you work directly with the people who built the business and understand the technology inside out.
Our founder-led model means faster decision-making, more flexible solutions, and a level of personal accountability that simply doesn’t exist in large, faceless corporations. You’re supported by real experts — not call centres — ensuring your system performs exactly as it should and your results speak for themselves.
We believe in our systems so much that we make it easy to try them without risk. Whether you prefer to rent, buy, or rent-then-buy, you have the freedom to find what fits best for you.
Our goal is simple — to make advanced wellness technology accessible. You can spread payments over 12 months through our trusted finance partner, or choose our 3-month in-house payment option directly with Oxydise.
Every plan is fully transparent — no hidden fees, no long applications — just straightforward options that reflect our confidence in the equipment and our commitment to your results.
Every Oxydise system — from red-light panels to HBOT chambers — meets CE and UKCA standards and complies with ISO 9001, 14001, and 45001 certifications. Each unit is independently pressure-tested, electrically inspected, and safety-verified before leaving our facility.
Our 1.5 ATA chambers are pressure-tested to 1.75 ATA, and our 2.0 ATA hard-shell units are tested to 3.0 ATA — well above their normal operating range — to ensure exceptional structural integrity and long-term reliability.
Our expertise is anchored by real credentials — Alan Trim, Oxydise Co-Founder, is certified by the International Board of Undersea Medicine (IBUM), bringing clinical insight and hands-on experience to every client protocol. Our Clinical Board, chaired by Oli Patrick, oversees best-practice standards across all Oxydise programmes, ensuring every protocol aligns with the latest evidence in recovery and wellness. Dr Masha, a certified HBOT specialist, leads our HBOT Safety Training and Certification Course, giving every client and practitioner complete confidence in correct, safe operation.
We take contraindications seriously — from screening and consultation to ongoing use, safety always comes first. When we deliver your system, our team assembles it, performs full functional checks, and provides hands-on training so you know exactly how to use it from day one.
At Oxydise, our relationship doesn’t end when your system arrives — it begins there. Every client receives personalised guidance and structured training to ensure their chamber or red-light system is used safely, confidently, and effectively from day one.
Your induction is delivered by trained Oxydise technicians, who assemble the system on-site, perform full safety checks, and walk you through correct operation and maintenance. Beyond setup, you’ll have access to ongoing clinical and technical support, so you always know how to get the most from your system.
Our expertise is anchored by real credentials — Alan Trim, Oxydise Co-Founder, is certified by the International Board of Undersea Medicine (IBUM), bringing clinical insight and hands-on experience to every client protocol. Our Clinical Board, chaired by Oli Patrick, and our HBOT safety lead, Dr Masha, who delivers the Oxydise HBOT Safety and Certification Course, together ensure every programme reflects best practice and up-to-date science.
We take contraindications and safety seriously — every recommendation is designed to optimise results while protecting client wellbeing. And when you need help, we’re just a call away — direct access to real experts who know the equipment and the science behind it.
All Oxydise systems are stocked, assembled, and serviced here in the UK — so your experience is fast, seamless, and stress-free. There are no customs delays, import fees, or long lead times to worry about.
For our 1.5 ATA chambers, typical delivery and setup take around seven days, with installation arranged at your convenience. Hard-shell 2.0 ATA systems may take slightly longer due to logistics and final testing, but our team will always give you a clear, realistic delivery window.
When your system arrives, our trained technicians deliver, assemble, and test everything on-site, then walk you through safe operation and usage protocols before handing it over. If you have specific timing needs, you can always call us directly — we’ll do everything possible to accommodate your schedule and ensure a smooth start to your wellness journey.
Every Oxydise system comes with a 2-year comprehensive warranty as standard — reflecting the confidence we have in our build quality and testing. If an issue ever arises, our process is straightforward and fast.
Once a fault is reported, our team will assess the problem the same day and decide whether a repair or full replacement is the best course of action. In most cases, issues are resolved within three days — minimising disruption to your recovery or wellness routine.
We have a dedicated HBOT engineer on our team who can diagnose and fix most issues quickly. If on-site repair isn’t possible, we’ll arrange a rapid unit replacement to get you back up and running without delay.
With Oxydise, you’re never left waiting — just direct access to the people who built, tested, and stand behind every system we deliver.